By Teresa Mauk, MSN, RN and Shanna R. Ingram, BSN, RN
Last month, the National Council of State Boards of Nursing (NCSBN) held their annual NCLEX® Conference, which provided a much-anticipated deeper look at the Next Generation NCLEX (NGN) project. Our educators joined thousands of others from around the United States and Canada as the NCSBN unveiled further details about the project, including a discussion about additional item types and scoring.
At UWorld, our nursing department is in the process of creating new NGN-style content to support students and faculty in this transition. We are excited about the opportunities the new item types provide for creating more robust, realistic clinical scenarios that support the development and evaluation of clinical judgment.
We know that these changes create anxiety for both students and faculty. However, a closer look at the NCSBN Clinical Judgment Measurement Model (CJMM), the framework utilized to develop NGN questions and measure clinical judgment, reveals its similarity to the Nursing Process and theories often used in nursing education.
The NCSBN utilized ideas from three cognitive theories–intuitive/humanistic (Benner, 1982; Tanner, 2006), cognitive continuum (Harbison, 2001), and information processing (Oppenheimer & Kelso, 2015)–to arrive at a definition for clinical judgment. Clinical judgment is “the observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solution in order to deliver safe client care.”
To better understand clinical judgment and its evaluation, the NCSBN created a flow chart outlining this process and its components–the Clinical Judgment Measurement Model.
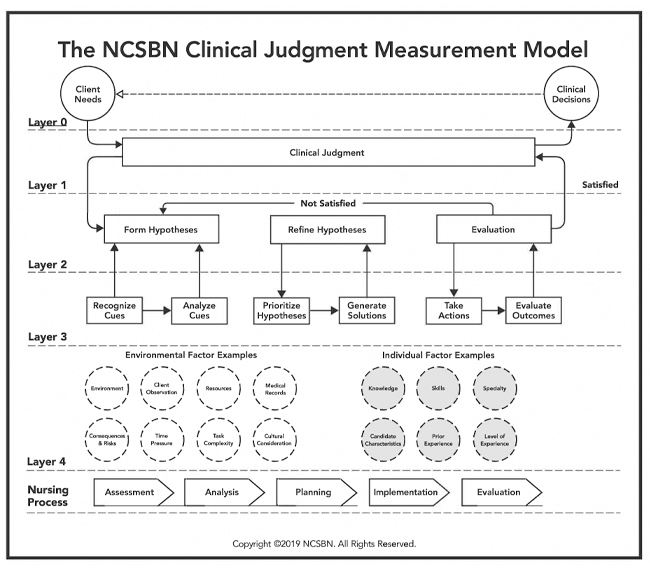
The focus of NGN questions is on Layer Three of the CJMM. Candidates will be provided an evolving case study and asked to answer one question for each of the six steps in Layer Three of the CJMM.
Let’s take a closer look at the six steps of Layer Three to better understand what is being asked of learners:
1. Recognize cues within the provided case study and data
The first step learners must successfully complete when making clinical decisions is to recognize cues present in the clinical environment, also known as situational awareness. In this step, learners must weed through the vast amount of clinical data available about a client (eg, vital signs, objective statements) as well the environment (eg, available resources based on level or type of care) and decide to which it is most important to attend. For example, learners may be asked to select the top four most important findings from a list of signs and symptoms.
As experienced nurses, we are able to quickly analyze a client’s lab results, vital signs, and other subjective and objective data to determine which of the information we need to act upon first. However, research has shown that learners struggle with situational awareness and tend to prioritize task completion rather than prioritizing according to client needs. Therefore, it is important for nursing faculty to help students understand how to interpret and organize clinical cues.
In the classic work Educating Nurses: A Call for Radical Transformation, Benner describes the importance of learning in context. In order for learners to develop the ability to recognize cues, they must be presented with clinically-realistic situations in which they can practice recognizing salient cues.
2. Analyze cues and data to form hypotheses about potential concerns
In this step of the CJMM, the learner must determine what the cues are suggesting about the client’s situation and formulate hypotheses about potential health alterations and disease processes.
The learner must categorize and analyze the information (cues, objective and subjective data) to determine how the information supports their hypotheses, realizing that some signs and symptoms (e.g., fever and fatigue) may be common to several hypotheses.
3. Choose the priority concern from the hypotheses
In step two, the learner considered how the findings related to various hypotheses. Next, the learner must organize the various hypotheses to determine which is the priority client concern. For example, the learner may have to decide what complications are most likely to arise from the health alteration or which data puts the client most at risk.
4. Plan solutions that will improve the priority concern
After the priority concern is determined, the learner must determine how to act or generate solutions for the concern. This is the equivalent of developing a plan of care. In this step, learners may be asked to decide if an intervention is indicated or contraindicated for the client.
5. Identify appropriate actions to achieve the solution
Now that the client’s plan of care is complete, the nurse must take action. We know that standard order sets contain many different actions with varying levels of importance. Here, the learner must determine which actions will be taken or prioritized. Taking action has a very broad meaning here as the nurse may need to further assess or monitor the client or recommend a higher level of care.
6. Evaluate for expected improvements and outcomes
Finally, the learner must determine if the nursing actions or interventions implemented in step five resulted in the expected client outcomes. For example: Did the client’s blood pressure decrease after the nurse administered an antihypertensive? Was the client able to rest after minimizing environmental stimulation?
Nurses’ ultimate goal is to improve the client’s well-being. Without evaluation, the nurse will not know if the intervention was successful in meeting client outcomes.
In summary, the critical learner processes that demonstrate clinical judgment include:
- Interprets data quickly and recognizes cues
- Analyzes and organizes cues into hypotheses about potential concerns
- Fleshes out the priority hypothesis (what is urgent and what can wait)
- Understands solutions required to improve the priority concern
- Uses essential knowledge to identify appropriate nursing interventions for expected outcomes
- Evaluates for improvement in condition, and continues or adjusts care as indicated
Although it may seem intimidating at first, the CJMM closely aligns with the nursing process, a theory nurse educators understand and apply regularly. It is important that educators spend some time familiarizing themselves with the new terminology and item types utilized in NGN. Consulting the CJMM will help guide content creation and align evaluation methods with clinical judgment in the style of the Next Generation NCLEX.
Developing learners’ clinical judgment and reasoning skills takes deliberate practice. Here are a few useful techniques nurse educators can implement now to begin transitioning to the CJMM and support the development of clinical judgment:
- Frequent use of prepared case studies (complete or unfolding) in the classroom
- A class exercise in which learners develop a case study about a topic
- Concept mapping to visually represent the relationship between multiple topics
- Use of mind maps to visualize and organize information about a central topic
- Developing ‘what if’ scenarios about a single case study that lead to different outcomes. Have small groups of learners develop the various scenarios for presentation.
- Having learners ‘think aloud’ in clinical situations to clarify their reasoning and for instructor feedback. This is particularly useful if initiated early in a nursing program.
- Written reflections following simulations or clinical care experiences that focus on what worked and at least one ‘what if’ scenario
- Having learners compare and contrast clinical data and interventions for two clients with the same diagnosis during a clinical experience (e.g., two clients with COPD, atrial fibrillation, or heart failure). Were the clients’ admitting symptoms the same? How did treatment differ? Were medications the same or different? How did client outcomes compare? *Note: The learner does not have to be providing care for both, or either, of the clients; this exercise can be completed using a review of data in the clients’ electronic medical records.
With expanding technology and increasing client acuity, it is critical that learners develop sound clinical reasoning and judgment. We must teach our learners to ‘think like a nurse’; our clients are counting on it!
References
1. Betts, J., Muntean, W., Kim, D., Jorion, N., & Dickison, P. (2019). Building a Method for Writing Clinical Judgment Items for Entry-Level Nursing Exams. Journal of Applied Testing Technology, 20(S2), 21–36. http://www.jattjournal.com/index.php/atp/article/view/143674