Family Nurse Practitioner (FNP)
Sample Questions
Practicing with exam-style sample questions is the most effective way to prepare for ANCC® and AANP® exams, because if practice feels like the actual exam, then the real thing will feel like practice.
High-Quality FNP-Style Practice Questions
Our FNP practice questions are aligned to the FNP Examination Blueprint and developed by our in-house team of Nurse Practitioners to meet or exceed exam-level difficulty.
Benefit from
Exam-Like Practice
Learn From
Detailed Rationales
Customize Tests
to Your Needs
Free Family Nurse Practitioner Sample Questions
Our FNP practice questions include innovative, content-rich rationales, paired with vivid illustrations and images to detail the clinical reasoning behind the correct and incorrect answers. Try some out for yourself:
A 21-year-old woman comes to the office for evaluation of urinary frequency and urgency for the past 2 days. She has also noticed scant vaginal discharge. The patient has never had these symptoms before. A urine sample is obtained for urinalysis and culture. Which of the following additional findings would be most suggestive of a diagnosis of pyelonephritis?
| A. Bacteriuria | ||
| B. Leukocytosis | ||
| C. Microscopic hematuria | ||
| D. White blood cell casts |
Explanation:
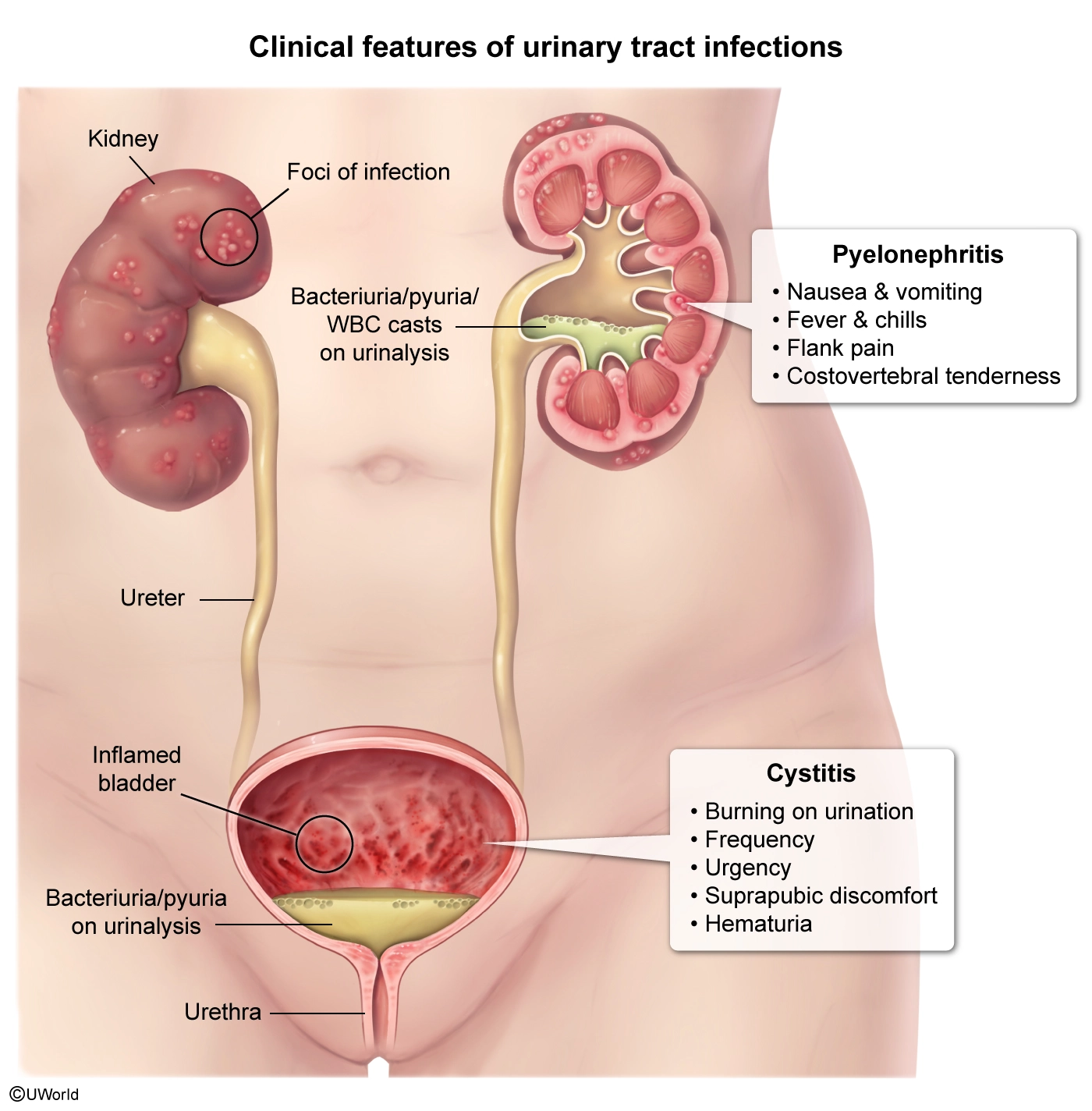
This patient has urinary frequency and urgency consistent with a urinary tract infection (UTI). Women are more susceptible to UTIs because the female urethra is closer to the rectum and shorter than the male urethra. Sexual intercourse is often a precipitating factor because it introduces enteric bacteria to the periurethral area, leading to ascending infection of the bladder.
UTIs are categorized into either upper (eg, pyelonephritis) or lower (eg, cystitis) infections based on the ascension of bacteria through the urinary tract. Pyelonephritis and cystitis can share concomitant clinical features including dysuria, suprapubic pressure, and hematuria. Urinalysis with microscopy is often performed to confirm the diagnosis of UTI, but both upper and lower UTIs can show hematuria, pyuria (presence of urine white blood cells [WBCs]), and bacteriuria (Choices A and C).
However, the presence of WBC casts on urinalysis differentiates between upper and lower UTIs and can confirm the diagnosis of pyelonephritis. This is because WBC casts are formed only in renal tubules, where WBCs precipitate with a protein secreted by tubular epithelial cells. WBC casts can also be seen with other intrarenal disorders (eg, acute interstitial nephritis), but urinary frequency and urgency are not typically present.
(Choice B) Leukocytosis is a nonspecific sign indicating systemic inflammation. Although, usually present with pyelonephritis and absent with lower UTIs (eg, cystitis), it may occur in numerous other conditions (eg, pelvic inflammatory disease). In contrast, urine WBC casts are specific for intrarenal pathology.
Educational objective:
Both upper (eg, pyelonephritis) and lower (eg, cystitis) urinary tract infections (UTIs) can show microscopic hematuria, pyuria, and bacteriuria on urinalysis with microscopy. However, the presence of white blood cell (WBC) casts can confirm the diagnosis of pyelonephritis in patients with UTI symptoms because WBC casts form only in the renal tubules.
A 55-year-old man with type 2 diabetes mellitus presents with severe right foot pain that started suddenly in the middle of the night after he had a steak dinner with friends. Physical examination shows swelling and tenderness of the first metatarsophalangeal joint. Joint aspiration is performed, and microscopic findings from the synovial fluid reveal the presence of monosodium urate crystals. Which of the following is the best initial treatment?
| A. Allopurinol | ||
| B. Non-steroidal anti-inflammatory drugs (NSAIDs) | ||
| C. Prednisone | ||
| D. Probenecid |
Explanation:
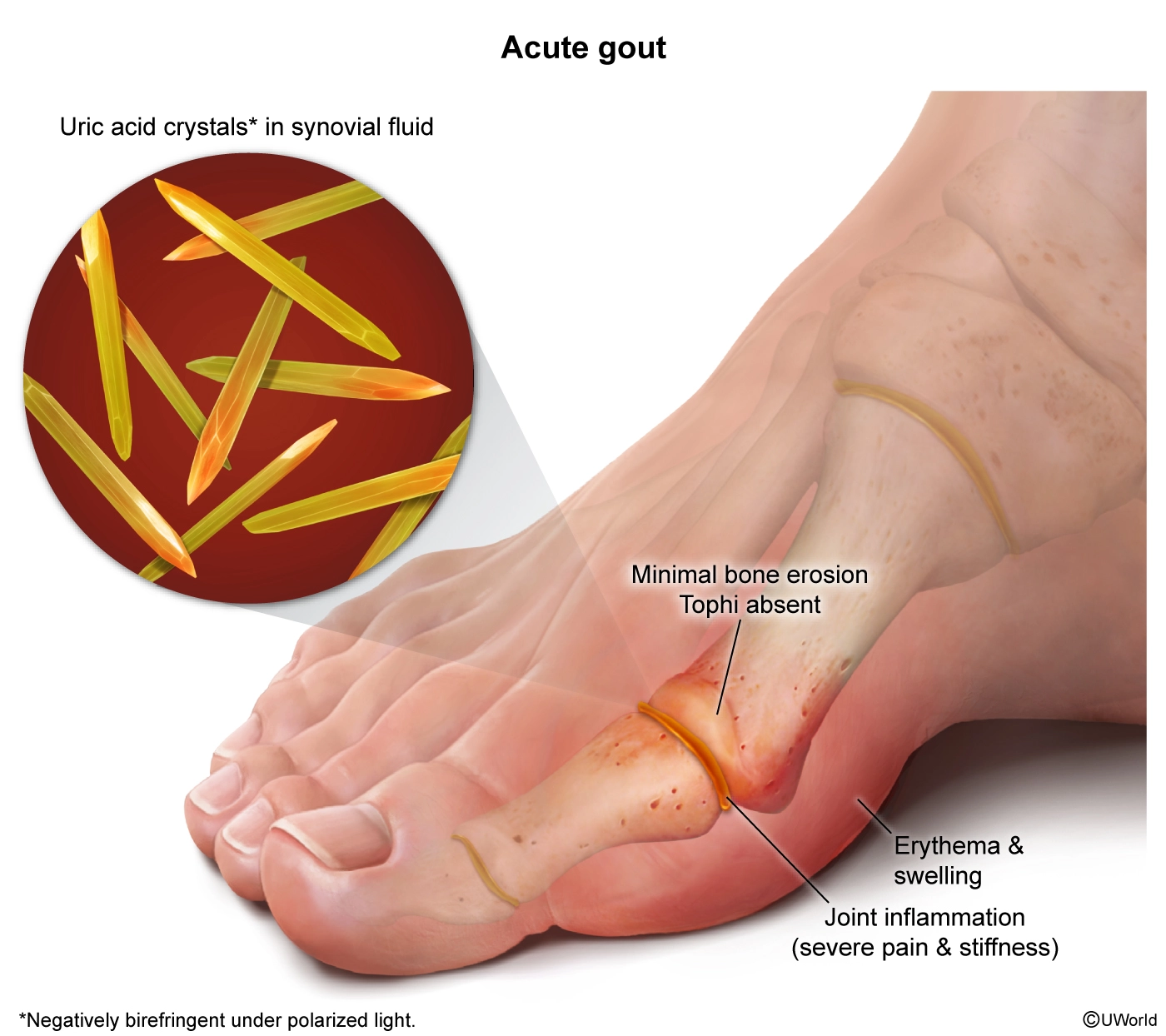
This patient with acute monoarthritis of the metatarsophalangeal joint and a synovial fluid analysis showing monosodium urate crystals (observed as needle-shaped, negatively birefringent crystals under polarized light) has gout. Gout attacks can be precipitated by conditions that cause increased production or decreased elimination of uric acid or an acute change in uric acid levels. Common triggers include heavy alcohol consumption, intake of urate-rich foods (eg, steak), trauma/surgery, dehydration, and medications that raise (eg, thiazide diuretics) or lower (eg, allopurinol) uric acid levels.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a first-line treatment for most patients with acute gouty arthritis. They inhibit cyclooxygenase enzymes and therefore decrease prostaglandin synthesis and exert a broad anti-inflammatory effect that includes inhibition of neutrophils. NSAIDs should be avoided in patients with renal and hepatic dysfunction or those at high risk for peptic ulcer.
(Choices A and D) Uric acid–lowering therapy with either uricosuric agents (eg, probenecid) or xanthine oxidase inhibitors (eg, allopurinol, febuxostat) is used to prevent acute attacks in patients with recurrent and progressive gouty arthritis and those with macroscopic tophi. These drugs should not be initiated during an acute gout attack because they can exacerbate acute arthritis.
(Choice C) Glucocorticoid therapy, either systemic or intraarticular, is used in patients with acute gout, and is preferred in those with contraindications to both NSAIDs and colchicine (eg, renal dysfunction, the elderly. However, this patient has diabetes mellitus, and glucocorticoid use would increase his blood glucose levels.
Educational objective:
Nonsteroidal anti-inflammatory drugs are the first-line treatment for acute gouty arthritis. They inhibit cyclooxygenase and therefore decrease prostaglandin synthesis and exert a broad anti-inflammatory effect that includes inhibition of neutrophils.
A 50-year-old man comes in for evaluation of hypersomnolence. The patient has been falling asleep at his desk at work and frequently falls asleep at home while watching his favorite television show. He works a standard 40-hour week as a systems analyst and regularly gets 8 hours of sleep a night. The patient reports drinking a daily cup of coffee on the way to work in the morning to help him “wake up” and a second late in the afternoon. Medical history includes hypertension. Blood pressure is 160/100 mm Hg and BMI is 38 kg/m2. Heart, lung, and neurologic examinations are normal. Which of the following is the best next step in management?
| A. Ambulatory ECG monitoring | ||
| B. CT scan of the head | ||
| C. Nocturnal polysomnography | ||
| D. Sleep hygiene education |
Explanation:
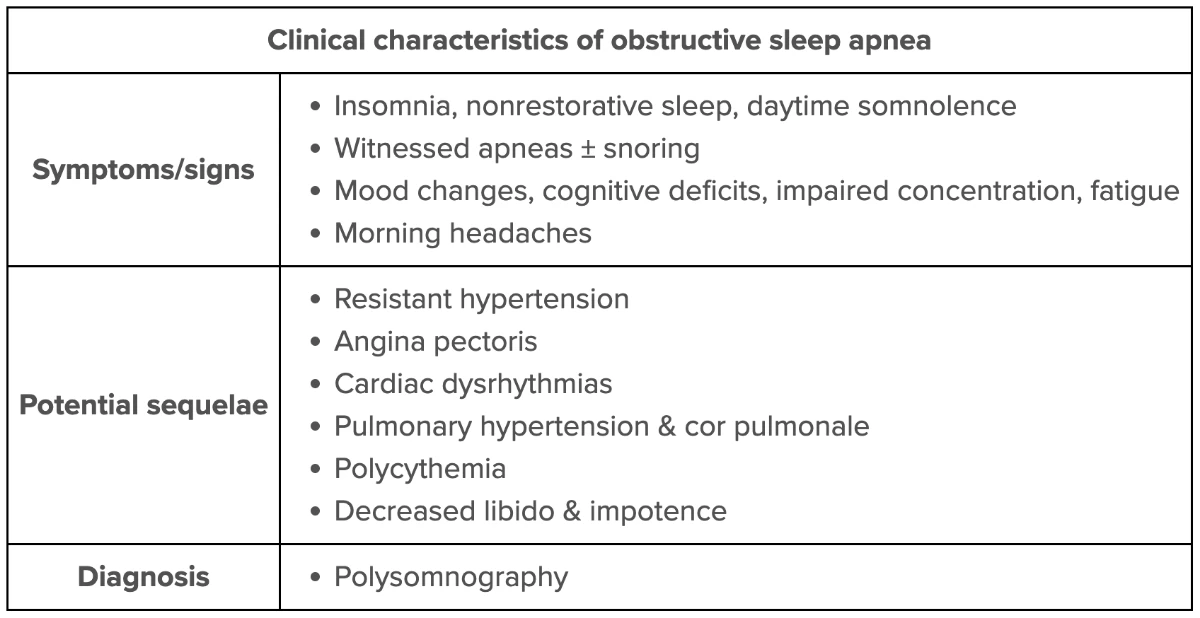
This patient with hypersomnolence (despite a sufficient sleep period [ie, 7-9 hr]), obesity, and no obvious behavioral risk factors for daytime sleepiness (eg, shift work, lengthy work hours) most likely has obstructive sleep apnea (OSA). OSA results from laxity of the pharyngeal musculature, leading to transient upper airway obstruction and nocturnal hypoventilation in the reduced-consciousness setting of sleep. These transitory obstructions cause frequent nocturnal arousals and disruptions in the normal sleep architecture, resulting in poor sleep quality and cumulative sleep insufficiency.
Typical manifestations of OSA-related sleep insufficiency include fatigue, excessive daytime sleepiness, falling asleep during sedentary daytime activities (eg, sitting at a desk at work, watching television), and frequent compensatory behaviors (eg, increased caffeine consumption). Patients with OSA will often exhibit restlessness during sleep with snoring and/or periods of apnea or gagging witnessed by bed partners. Morning headaches are frequently reported. Physical examination commonly demonstrates obesity (or increased neck girth) and resistant systemic hypertension, a multifactorial sympathetic response to hypoxemia and hypercapnia.
Patients with suspected OSA should be evaluated with overnight polysomnography (sleep study) to confirm the diagnosis. Symptoms are improved with positive pressure therapy. Alternate treatments include oral appliances (eg, mandibular advancement device) or surgical (eg, uvulopalatopharyngoplasty) interventions.
(Choice A) Intermittent cardiac arrhythmias can cause momentary lapses in consciousness (ie, syncope). However, this patient reports a clear history of falling asleep, not fainting, so ECG monitoring is not required.
(Choice B) A brain tumor or acute intracranial hemorrhage may present with symptoms of increased intracranial pressure (eg, hypersomnolence); however, this patient has no history of headache, head trauma, or neuro-focal deficits concerning for an intercranial lesion requiring a CT scan.
(Choice D) Discussions about good sleep hygiene should be included in the management of patients with difficulties falling or staying asleep (eg, insomnia). Sleep hygiene education is often inadequate when sleep insufficiency is due to poor sleep quality rather than insufficient quantity. This patient is currently sleeping well and regularly gets 8 hours of sleep each night.
Educational objective:
Obstructive sleep apnea is frequently implicated in hypersomnolence (excessive daytime sleepiness), especially in in individuals with risk factors (eg, obesity) and comorbid hypertension; nocturnal polysomnography should be ordered to confirm the diagnosis.
A 45-year-old man comes to the office for a routine preventive examination. He feels well but states that he has always had some dark spots on his back. Physical examination shows many pigmented lesions on the back, including a single, flat, dark, 9-mm lesion with irregular borders. Which of the following is the best next step in the management of this patient’s skin lesion?
| A. Excisional biopsy | ||
| B. Incisional biopsy | ||
| C. Photographic documentation and comparison in 6-12 months | ||
| D. Reassurance and routine follow up only |
Explanation:
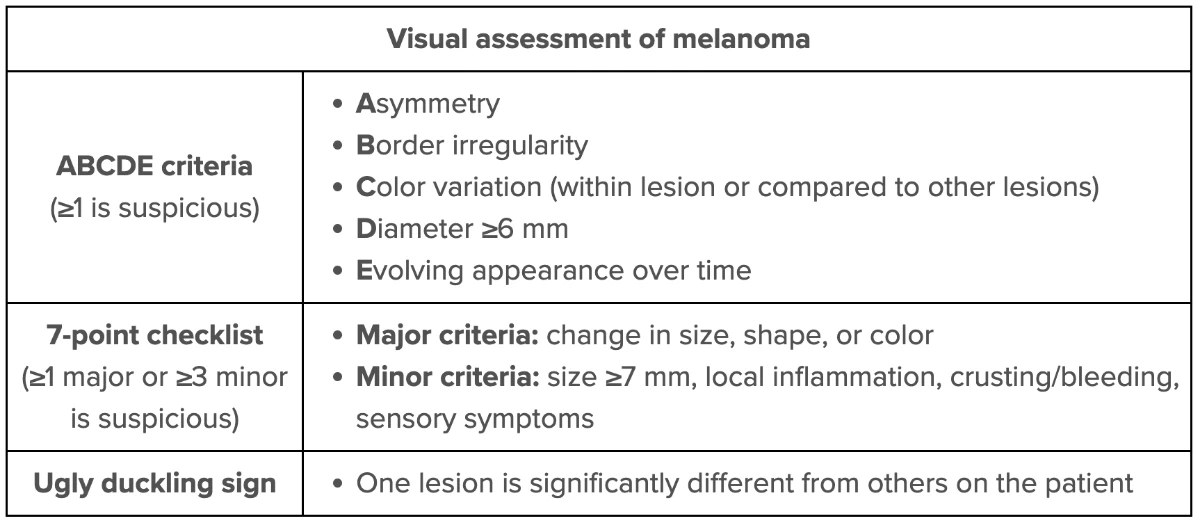
This patient’s suspicious pigmented lesion has an increased risk of malignant melanoma based on size (≥6 mm in diameter) and mild border irregularity. Other features that suggest melanoma include asymmetry, color variation, and change over time; some lesions may also have inflammatory changes, crusting/bleeding, or sensory abnormalities.
Due to the aggressive nature and high metastatic potential of melanoma, early referral to a specialist (eg, dermatologist) and definitive diagnosis with biopsy should be considered for any suspicious pigmented skin lesion. Lesion thickness is the most important prognostic determinant in melanoma (ie, increased tumor thickness decreases the survival rate). Therefore, an excisional biopsy with an elliptical technique is the preferred method and should include the entire lesion with a 1- to 3-mm margin. Patients with confirmed melanoma require additional resection and staging procedures, which should be performed within 4-6 weeks of diagnosis.
(Choice B) Incisional biopsy (in which only a portion of the lesion is removed) is not generally recommended for melanoma because it does not allow determination of lesion thickness. However, it may be considered for unusually large tumors or for locations where cosmetic results are important (eg, the face).
(Choices C and D) Periodic surveillance (with or without photographic documentation) is appropriate for patients with lesions that do not require biopsy (eg, symmetric, small) but are at risk for melanoma. This patient’s lesion requires immediate biopsy because of its diameter, evolution over time, and border irregularity.
Educational objective:
Patients with skin lesions suspicious for melanoma should have an excisional biopsy that includes the entire lesion with a 1- to 3-mm margin of surrounding skin and subcutaneous fat.
A 50-year-old man is evaluated for severe headache, nausea, and left eye pain. His symptoms started suddenly several hours ago, and his headache has not improved with rest and ibuprofen. He has had a mild cold and took an over-the-counter oral decongestant this morning. Physical examination shows a left pupil that is nonreactive and mid-dilated. The eye appears red with conjunctival flushing. Which of the following is the best next step in management?
| A. Eye patch placement and follow up in 3 days | ||
| B. Fluorescein staining of the eye | ||
| C. No additional management indicated | ||
| D. Tonometry |
Explanation:
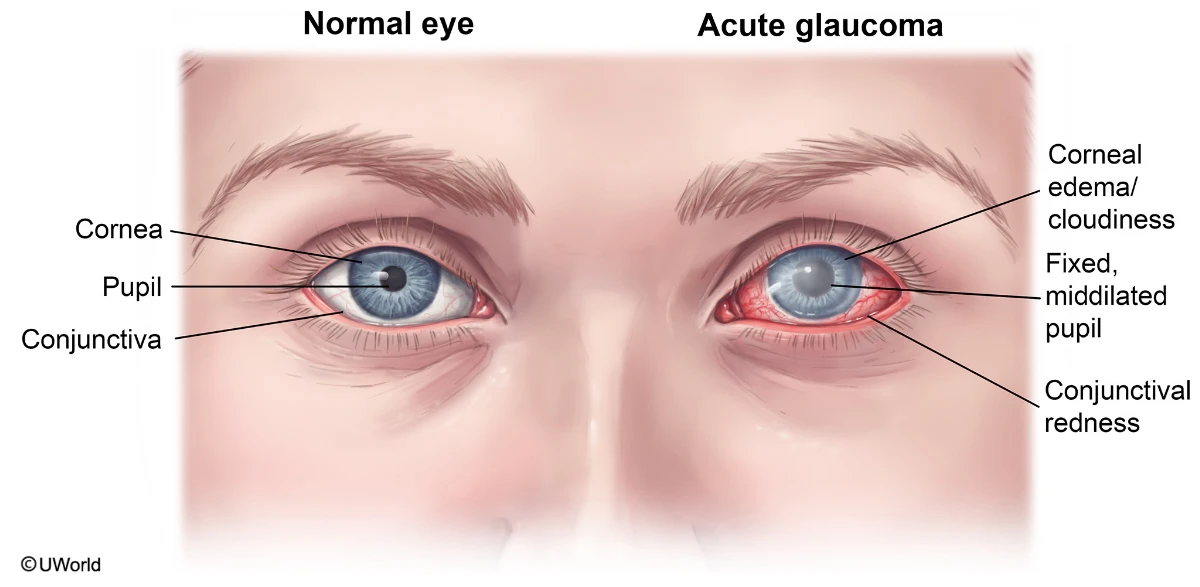
This patient most likely has acute angle-closure glaucoma (ACG), which results from a sudden onset of increased intraocular pressure due to impaired aqueous humor drainage through the angle of the anterior chamber. Acute ACG typically occurs spontaneously but may be triggered by certain medications (eg, decongestants, anticholinergics, antihistamines), as in this patient. As intraocular pressure increases, patients develop eye pain, headache, conjunctival redness, and a fixed, mid-dilated pupil that reacts poorly to light.
Patients with suspected acute ACG require immediate evaluation because the increased intraocular pressure leads to rapid damage to the optic nerve, potentially resulting in permanent vision loss (Choices A and C). In these patients, the best next step is tonometry, which can be used to confirm an elevated intraocular pressure. Patients also require an emergency ophthalmology referral for gonioscopy, which can be used to verify angle closure and is the gold standard in diagnosis.
(Choice B) Fluorescein staining of the eye is usually performed to detect corneal abrasions or herpes keratitis, which can cause a painful, red eye. These conditions are not usually associated with headache, nausea, and a fixed, mid-dilated pupil.
Educational objective:
Acute angle-closure glaucoma typically presents with a painful, red eye; headache; and a fixed, mid-dilated pupil and is due to an acute rise in intraocular pressure from impaired aqueous humor drainage in the anterior chamber. In patients with suspected angle-closure glaucoma, the best next step is tonometry and emergency ophthalmology referral.
A 62-year-old woman comes to the office due to a vague feeling of heaviness in her legs, especially when standing for long periods. The patient has worked as a cashier at a department store for the last 20 years and her symptoms are worst at the end of her work shift. Examination of both lower extremities shows dilated, tortuous veins at the calves and ankles bilaterally, with no erythema or edema. Upper extremity examination is unremarkable. This patient’s current condition increases the risk for which of the following?
| A. Intermittent claudication | ||
| B. Myocardial infarction | ||
| C. Pulmonary embolism | ||
| D. Venous stasis ulcers |
Explanation:
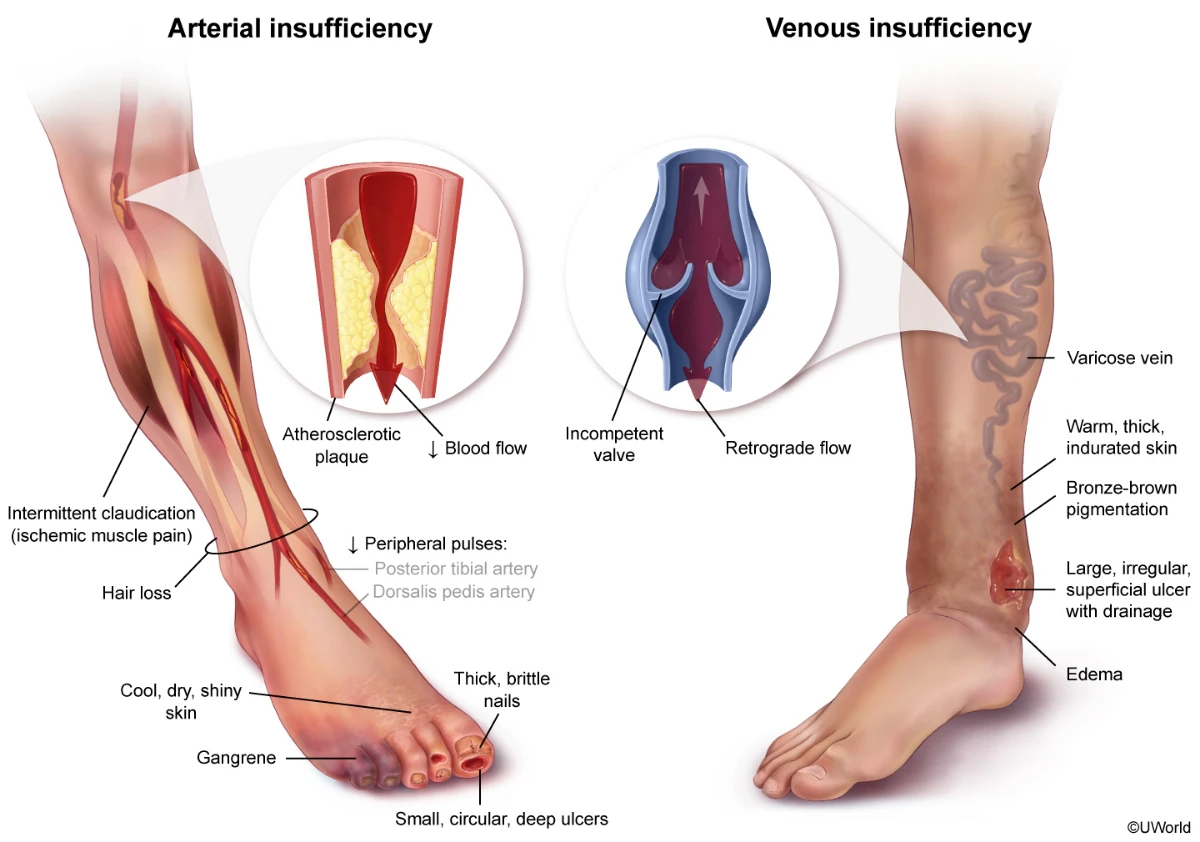
This patient has varicose veins – dilated, tortuous veins typically involving the superficial venous drainage of the leg. Increased intraluminal pressure or loss of vessel wall strength can lead to venous dilation and failure of the venous valves. The resulting backflow of blood exacerbates the venous hypertension, precipitating further valvular incompetence and venous congestion.
Varicose veins are most common in patients age >50, and the risk is increased by conditions that cause elevated venous pressure (eg, prolonged standing, pregnancy, obesity). There is also often a familial association, suggesting possible genetic factors involving the venous wall or valves. Common complications include chronic edema, stasis dermatitis, venous stasis ulcers, poor wound healing, and infection.
(Choices A and B) Intermittent claudication is achy or crampy pain in the legs caused by inadequate arterial blood flow, usually due to atherosclerosis in the branches of the femoral artery. In contrast to venous disease, in which the pain is worsened by prolonged standing or sitting with the legs dependent, claudication due to arterial disease is worse with exertion and relieved with rest. Because peripheral artery atherosclerosis is often associated with atherosclerotic disease elsewhere, patients with intermittent claudication have an increased risk for ischemic stroke and myocardial infarction.
(Choice C) Deep venous thrombosis of the lower extremity can lead to pulmonary embolism. Although varicose veins can sometimes be complicated by thrombophlebitis, it primarily involves the superficial rather than deep venous system and a clear risk for increased incidence of pulmonary embolism has not been established.
Educational objective:
Varicose veins are dilated, tortuous veins most commonly found in the superficial veins of the leg. They are caused by chronically increased intraluminal pressure and/or loss of tensile strength in the vessel wall, leading to incompetence of the venous valves. Common complications include edema, stasis dermatitis, venous stasis ulcers, poor wound healing, and infections.
A 36-year-old healthy man presents with intermittent episodes of rectal bleeding over the past 2 months. Initially, he noted only small streaks of blood on the tissue when wiping, but yesterday he dripped bright red blood after defecating and the stool was coated with blood. The patient has had no anal or abdominal pain, anorexia, weight loss, or changes in bowel pattern. The perianal skin shows no abnormalities. No mass or tenderness is palpable on digital rectal examination. Anoscopy reveals purplish mucosal bulges. Which of the following is the best next step in management?
| A. Biopsy of the anal lesions | ||
| B. High-fiber diet and follow-up | ||
| C. Referral for colonoscopy | ||
| D. Referral for surgical evaluation |
Explanation:
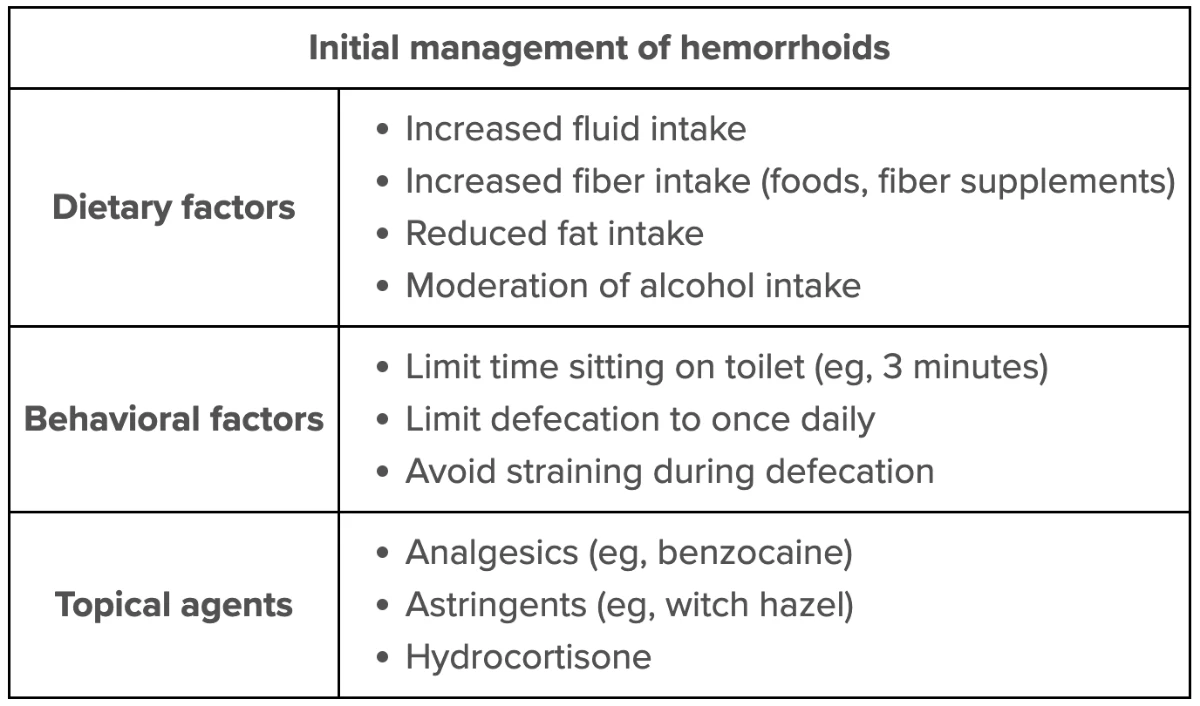
This patient has painless, bright red rectal bleeding and mucosal bulges on anoscopy consistent with internal hemorrhoids. Hemorrhoids are the most common cause of low-volume rectal bleeding, especially in patients who do not have red-flag features (eg, passage of dark blood or blood mixed with stool, fever, abdominal pain, change in bowel habits) to suggest more serious causes. The diagnosis is usually obvious based on clinical findings. Anoscopy is useful for those whose hemorrhoids are not palpable on examination, but further diagnostic testing is not usually required for young, otherwise healthy patients with typical symptoms, such as this patient.
Initial management of uncomplicated hemorrhoids includes increased intake of fluid and fiber (eg, psyllium husk), reduction in fat and alcohol intake, and regular exercise. Additional measures may include topical hydrocortisone, astringents (eg, witch hazel), and local anesthetics (eg, benzocaine, lidocaine). More aggressive management, including rubber band ligation and surgical hemorrhoidectomy, is generally advised only for patients with refractory symptoms or prolapsed hemorrhoids that cannot be reduced manually (ie, grade IV hemorrhoids) (Choice D).
(Choice A) Biopsy is warranted for pedunculated or sessile colorectal polyps, which typically present as pink, red, or flesh-colored papules or masses. The purplish bulges in this patient are typical for hemorrhoids, and biopsy would lead only to unnecessary bleeding.
(Choice C) Colonoscopy is recommended for patients who have profuse rectal bleeding or who are at high risk for colorectal cancer. High risk features include prior adenomatous colon polyps, age ≥50, age 40-49 with a first-degree relative with colorectal cancer at age <60, or a familial colon cancer syndrome (eg, Lynch syndrome). Younger patients, such as this patient, with low-volume bleeding and a benign explanation (eg, hemorrhoids) may be monitored without colonoscopy.
Educational objective:
Initial management of uncomplicated hemorrhoids includes increased intake of fluid and fiber, reduction of fat and alcohol intake, and regular exercise. Rubber band ligation and surgical hemorrhoidectomy are advised only for patients with refractory symptoms or prolapsed hemorrhoids that cannot be reduced manually.
A 26-year-old woman, gravida 2 para 1, at 37 weeks gestation is admitted to the hospital in active labor. She receives an epidural and slowly progresses to complete cervical dilation. The patient pushes for 2 hours; the fetal head delivers, immediately retracts into the perineum, and the anterior shoulder does not deliver. Which of the following is the greatest risk factor for this patient’s clinical presentation?
| A. Fetal gestational age | ||
| B. Maternal age at delivery | ||
| C. Maternal chronic hypertension | ||
| D. Maternal type 2 diabetes mellitus |
Explanation:
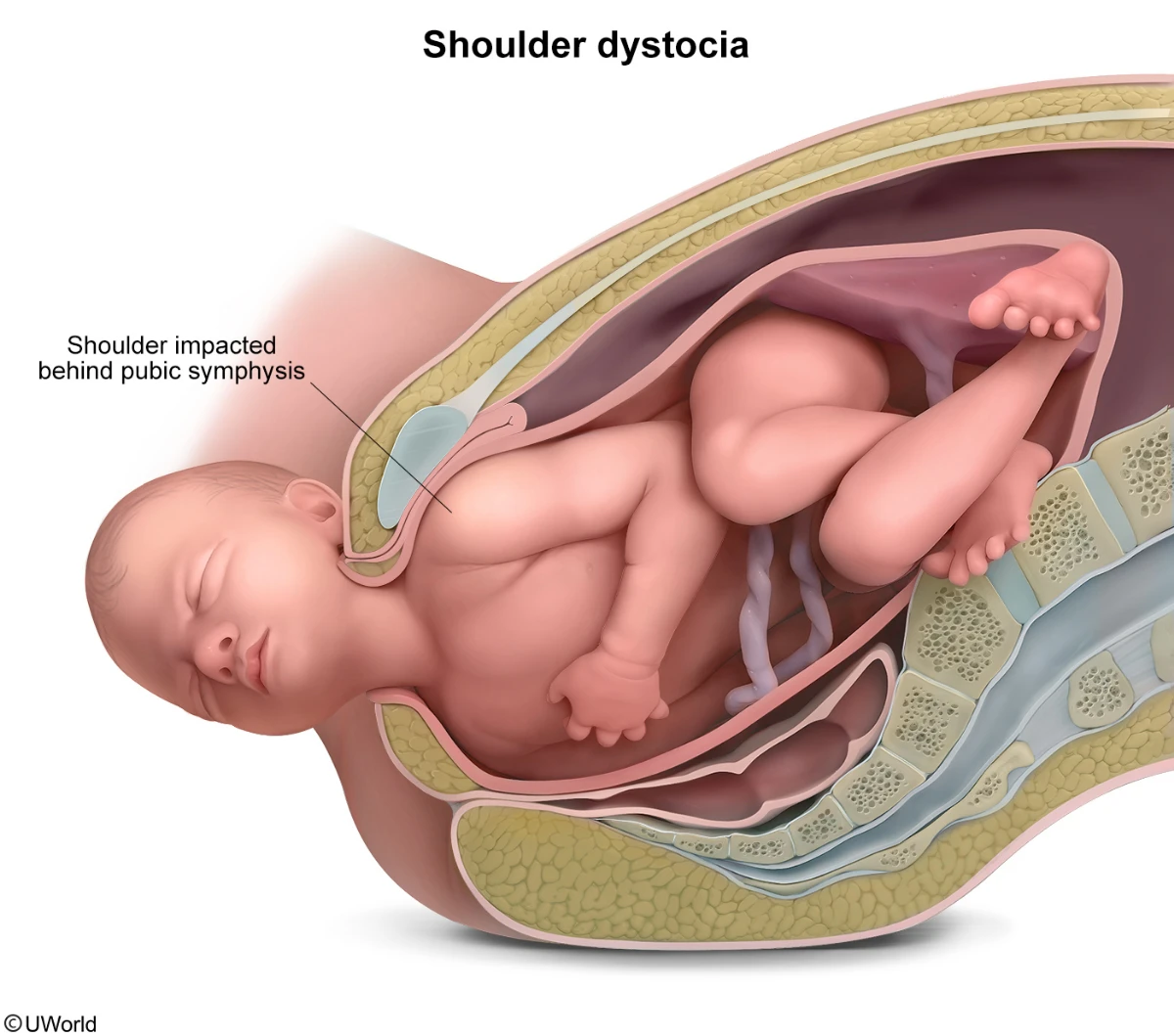
Shoulder dystocia occurs when the fetal shoulders become impacted behind the maternal pubic symphysis. In patients with shoulder dystocia, the fetal head retracts into the maternal perineum after it delivers (“turtle sign“) and the anterior fetal shoulder does not deliver with the usual obstetric maneuvers (eg, gentle downward traction).
Shoulder dystocia is an obstetric emergency because prolonged umbilical cord compression while the fetus is in the birth canal can result in hypoxemia and its complications (eg, hypoxic encephalopathy, death). Maneuvers involved in the management of shoulder dystocia can result in additional neonatal complications including brachial plexus injury and clavicular or humeral fracture. Maternal complications include perineal laceration and postpartum hemorrhage.
Risk factors for shoulder dystocia include conditions associated with fetal macrosomia such as maternal obesity, excessive maternal weight gain, and ≥42 weeks (post-term) gestation (Choice A). Patients with gestational or pre-gestational diabetes mellitus are at high risk for shoulder dystocia due to an association with fetal macrosomia and with truncal asymmetry (the disproportionate enlargement of the fetal shoulders and trunk compared to the head). Truncal asymmetry increases the likelihood that after the fetal head delivers with the usual obstetric maneuvers, the shoulders do not.
(Choice B) Advanced maternal age (age ≥35) is associated with an increased risk of shoulder dystocia; however, this is likely due to the increased risk of pregnancy-related co-morbidities (eg, diabetes mellitus).
(Choice C) Chronic hypertension is associated with fetal growth restriction rather than fetal macrosomia and therefore is not associated with shoulder dystocia.
Educational objective:
Shoulder dystocia, the impaction of the fetal shoulder behind the maternal pubic symphysis, presents as the retraction of the fetal head into the maternal perineum immediately after it delivers. Risk factors include conditions that cause fetal macrosomia such as maternal diabetes mellitus, maternal obesity, and post-term (≥42 weeks) gestation.
Pass the FNP with Exam-Like Practice!
We are committed to providing you with only the best questions and explanations. Our FNP practice questions include the hallmark features that have helped over a million nurses succeed.
UWorld Nursing FNP Student Testimonials
We measure the success of our test prep products by the success of our users. Here’s what UWorld Nursing students are saying:
The rationales are thorough and explain not only why you are right, but also why the other options are wrong. Really great for synthesizing the information, not just memorizing it. The images and graphics are also very helpful - especially for conditions one might not see during school placements.”
I've really enjoyed not only the variety of questions, but also the ability to highlight and mark questions so you can go back to it. It is extremely helpful in explaining why an answer is not correct. It gives you hints and highlights to help with how to read the questions and answer them.”
I really appreciate the thorough explanations providing rationale for why each possible answer selection is correct or incorrect. These include pictures, audio recordings, graphs, tables, etc. VERY helpful for studying.”