What is Clinical Judgment?
Clinical judgment is a term that's commonly used in nursing, but defining it can be somewhat tricky. Ask 5 experienced nurses what clinical judgment is, and you'll likely get 5 different correct answers. In essence, clinical judgment is the ability to make informed, evidence-based decisions in patient care by recognizing key information, interpreting its significance, and taking appropriate action.1 It's the foundation of safe, effective nursing practice and a skill every nursing student must master.
With the introduction of the Next Generation NCLEX (NGN®), clinical judgment has taken center stage in nursing education and assessment. The National Council of State Boards of Nursing (NCSBN) developed the Clinical Judgment Measurement Model (CJMM) to better evaluate nursing candidates' readiness for real-world practice.2 The NGN uses this model to assess how well students can think critically and apply their knowledge in complex, evolving scenarios.
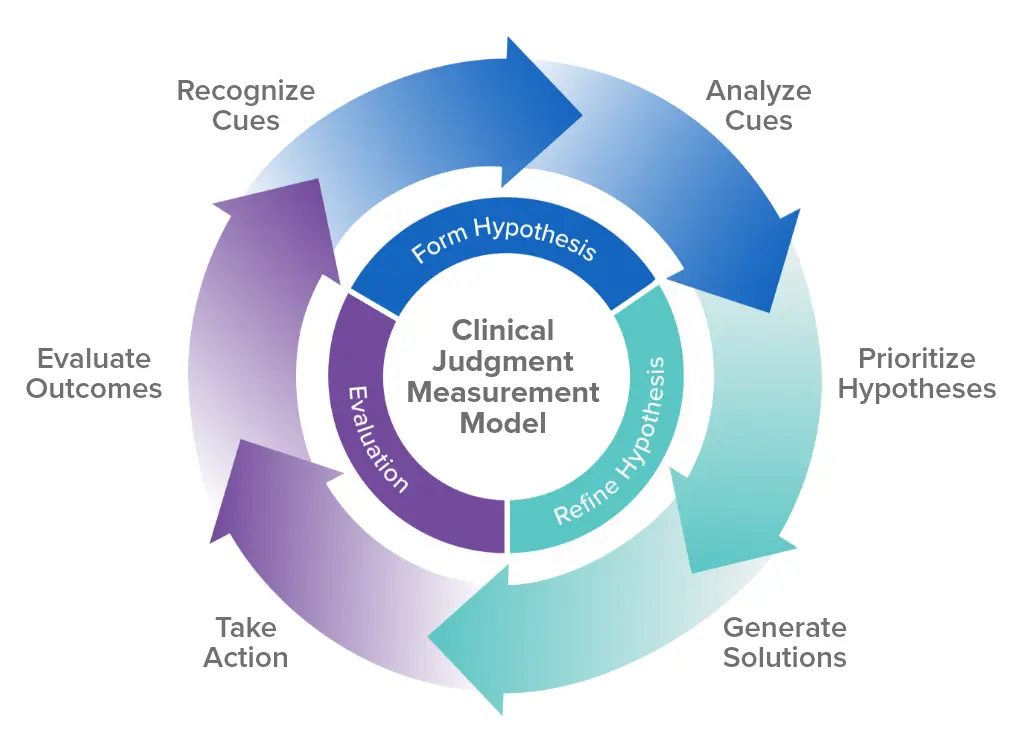
The CJMM breaks clinical judgment into 6 measurable steps:
- Recognize Cues: Identify the most critical pieces of information about a patient's condition.
- Analyze Cues: Determine what those cues mean in the context of the patient's overall health.
- Prioritize Hypotheses: Decide which issues are most urgent or pose the greatest risk.
- Generate Solutions: Develop potential interventions to address the priority issues.
- Take Action: Implement the chosen interventions.
- Evaluate Outcomes: Assess whether the interventions improved the patient's condition.
Recognize Cues
Recognizing cues is about identifying key pieces of information in a patient's condition that may indicate a change or potential concern. Whether it's noticing a shift in vital signs or observing subtle behavioral changes, the ability to recognize relevant cues is essential for effective clinical judgment.
For example, a nurse might detect a rapid heart rate and increased confusion in a patient, signaling a potential complication. Developing this skill in nursing students ensures they can gather the necessary information to make well-informed, critical decisions.
Analyze Cues
Once cues are recognized, the next step is to analyze their significance. This requires critical thinking, as your students must evaluate the patient's symptoms, medical history, and clinical data to form a clear picture of the patient's condition. For instance, if a patient has low blood pressure and an increased respiratory rate, students must analyze these cues to determine if the patient is at risk for shock. Strengthening the ability to analyze cues enhances students' clinical judgment by teaching them how to connect data to potential diagnoses.
Prioritize Hypotheses
In a clinical setting, it's important to determine what's urgent and what needs immediate attention. Prioritizing hypotheses is the process of ranking possible patient issues based on severity and urgency. For example, a nurse may have to decide whether to prioritize treating a patient's respiratory distress over other symptoms. Teaching your students how to prioritize problems develops their clinical judgment, enabling them to focus on the most pressing concerns while maintaining an organized approach to patient care.
Generate Solutions
Generating solutions involves identifying appropriate interventions that address the patient's condition. This step requires critical thinking and sound clinical judgment, as students must decide which actions will best resolve the issue based on the data they've analyzed. For instance, after recognizing dehydration in a patient, students may decide that administering IV fluids is the best course of action. Training your students to generate evidence-based solutions improves their ability to make effective, timely decisions in clinical practice.
Take Action
Taking action is the implementation phase where nurses carry out the interventions that have been identified. This step requires confidence, clinical expertise, and sound judgment to ensure the actions are appropriate for the patient's condition. For example, after diagnosing a patient with respiratory distress, a nurse might immediately administer oxygen and monitor the patient's response. Teaching your students to take decisive, evidence-based actions strengthens their clinical judgment and prepares them for real-world practice.
Evaluate Outcomes
Evaluating outcomes is the final step in the clinical judgment process, where nurses assess whether the interventions taken were effective in improving the patient's condition. This requires reflective critical thinking, as students must determine whether the goals were met and what adjustments, if any, need to be made. For instance, after administering IV fluids, a nurse would evaluate the patient's vital signs to see if they have stabilized. Encouraging your students to reflect on outcomes enhances their ability to make continuous improvements in patient care.
These steps are now embedded in NGN exam questions, including realistic unfolding case studies and new question types such as drag-and-drop and bow-tie formats. This approach tests knowledge and evaluates a student's ability to interpret data, prioritize care, and make sound clinical decisions.4
Clinical Judgment and Nursing Accreditation
Clinical judgment also plays a crucial role in nursing accreditation. Many accrediting bodies, such as the Accreditation Commission for Education in Nursing (ACEN) and the American Association of Colleges of Nursing (AACN), require programs to demonstrate how they are developing and assessing students' clinical judgment skills.5 Tools such as the CJMM provide a framework for integrating clinical judgment throughout nursing curricula, from simulated scenarios to real-world clinical experiences. For nursing educators, this means focusing on debriefing, case studies, and reflective exercises to help students refine these critical abilities.
Developing clinical judgment is a journey. While novice nurses may rely on structured steps, experienced nurses often make decisions instinctively, guided by their knowledge and experience. For educators, the challenge lies in bridging this gap — helping students build a strong foundation for clinical judgment while preparing them to succeed on the NGN and, ultimately, in their careers.
Clinical Judgment vs. Critical Thinking and Clinical Reasoning
While clinical judgment, critical thinking, and clinical reasoning are interconnected, each has a distinct role in nursing practice. Together, they form the foundation for sound decision-making, enabling nurses to provide safe, effective, and individualized patient care.
Critical Thinking Skills
Critical thinking is the backbone of clinical judgment. It's the ability to analyze, question, and make informed decisions based on available information.2 In nursing, critical thinking is essential for providing high-quality patient care, as it helps nurses make sense of complex situations, prioritize tasks, and ensure patient safety.
Developing these skills in your nursing students requires engaging them in activities that challenge their thinking. For instance, case studies allow students to analyze real-world scenarios, while reflection on practice questions can help them understand why certain answers are correct or incorrect. Mock clinical practices, where your students act out case scenarios, also offer a safe space to practice critical thinking. Through these activities, students learn to analyze data, differentiate between relevant and irrelevant information, seek additional details, and ultimately draw valid conclusions.
Clinical Reasoning Skills
Clinical reasoning is the process of applying nursing knowledge to interpret data and respond with appropriate care.1 It involves making connections between a patient's symptoms, medical history, and clinical findings to determine the best course of action. Like critical thinking, clinical reasoning is vital because it enables nurses to prioritize patient needs and apply interventions that align with their condition.
Your nursing students can sharpen their clinical reasoning skills through case studies, reflection on practice questions, and role-playing scenarios. By working through these exercises, students learn to recognize important clinical cues, interpret their meaning, and decide on interventions that will lead to the best patient outcomes. Developing strong clinical reasoning is a key step in building solid clinical judgment.
Developing clinical judgment is essential for nursing students to navigate complex patient care, succeed on the NGN, and thrive in their careers. UWorld's Next Generation NCLEX Educator Resources are specifically designed to help educators build these critical skills. Created by nursing experts, these tools go beyond improving pass rates — they instill confidence and prepare students for real-world practice. With assignable questions, detailed explanations, realistic case scenarios, and performance tracking, UWorld empowers educators to create meaningful learning experiences that strengthen clinical judgment and equip future nurses for the demands of their profession.
References
- American Association of Colleges of Nursing. (n.d.). Clinical judgment. Retrieved from https://www.aacnnursing.org/essentials/tool-kit/domains-concepts/clinical-judgement
- National Council of State Boards of Nursing. (n.d.). Clinical judgment measurement model. Retrieved from https://www.nclex.com/clinical-judgment-measurement-model.page
- Nurse Plus. (n.d.). The six clinical judgment skills on the NCLEX NGN. Retrieved from https://nurse.plus/become-a-nurse/nclex-ngn-six-clinical-judgment-skills/
- IPASS Processing. (n.d.). The NGN clinical judgment measurement model. Retrieved from https://ipassprocessing.com/ngn-clinical-judgment-measurement-model/
- UbiSim. (n.d.). Next Gen NCLEX (NGN) and the clinical judgment model. Retrieved from https://www.ubisimvr.com/blog/next-gen-nclex-ngn-and-the-clinical-judgment-model
- PubMed. (2022). Clinical judgment development and evaluation in nursing education: A systematic review. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35158134/
- ATI Testing. (2024, September 10). Using simulation to build clinical judgment and more. Retrieved from https://www.atitesting.com/educator/blog/knowledge/2024/09/10/using-simulation-to-build-clinical-judgment-and-more
- PubMed. (2021). Exploring clinical judgment in nursing: A concept analysis. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33231867/
- National Council of State Boards of Nursing. (n.d.). Next Generation NCLEX (NGN). Retrieved from https://www.nclex.com/next-generation-nclex.page