Practice with NCLEX-Style Sample Questions
Practicing with high-quality Next Generation and NCLEX-style sample questions is the most effective way to prepare for the exam, because if practice feels like the actual exam, then the real thing will feel like practice.
Check out our free NCLEX sample questions below!
The Best NCLEX-Style Practice Questions
We are committed to providing you with only the best questions and explanations. Our NGN practice questions include the same hallmark features that have helped over a million nurses succeed – clinically-relevant content, vivid imagery and illustrations, and in-depth explanations for correct and incorrect answers.
Benefit from
Exam-Like Practice
Learn From
Detailed Rationales
Customize Tests
to Your Needs
Free NCLEX-Style Sample Practice Questions
The best way to become more familiar with NCLEX-style questions is by practicing them. You’ve been through nursing school, so you have the knowledge. Now you just need to apply it. Choose your exam below to answer a few exam style questions …
The questions on the NCLEX-RN are designed to test your critical thinking skills and ability to apply knowledge in real-world scenarios. Don’t waste time practicing low-level questions. Challenge yourself with our NCLEX-RN sample questions.
The nurse is caring for a client at 39 weeks gestation who is receiving an IV oxytocin infusion for induction of labor. The nurse notes recurrent late decelerations on the fetal monitor. Which of the following actions should the nurse take? Select all that apply.
| 1. Administer an IV fluid bolus | ||
| 2. Reposition the client laterally. | ||
| 3. Discontinue the IV oxytocin infusion. | ||
| 4. Prepare the client for an amnioinfusion. | ||
| 5. Apply abdominal vibroacoustic stimulation. |
Explanation:
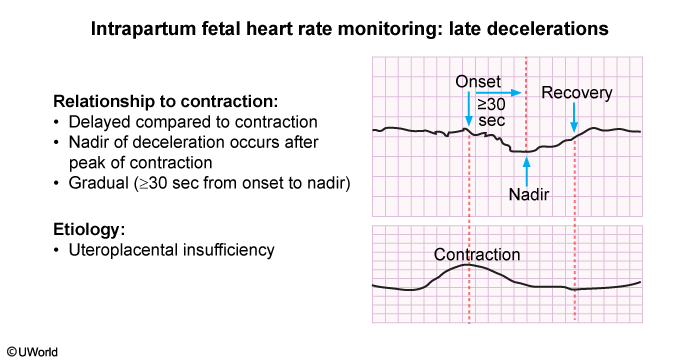
A late deceleration is a decrease in fetal heart rate (FHR) that occurs after the onset of a contraction and continues beyond its end. The lowest point (ie, nadir) occurs near the end of the contraction before the FHR gradually returns to baseline.
Late decelerations occur as a response to temporary fetal hypoxemia. Uteroplacental insufficiency, uterine tachysystole, and maternal supine hypotension are common causes because they compromise perfusion and oxygen availability to the fetus.
Intrauterine resuscitation interventions include:
-
Administering an IV fluid bolus to increase maternal blood volume (Option 1)
-
Repositioning the client laterally to relieve compression of the maternal inferior vena cava, which can be occluded by the weight of the gravid uterus when supine (Option 2)
-
Discontinuing the IV oxytocin infusion to reduce uterine stimulation and decrease contraction frequency; relaxation of the uterus increases uteroplacental blood flow and fetal oxygenation (Option 3)
(Option 4) An amnioinfusion (ie, instillation of fluid into the uterine cavity) is indicated to relieve persistent, recurrent variable decelerations caused by umbilical cord compression.
(Option 5) Vibroacoustic stimulation is used during nonreactive nonstress testing (ie, no accelerations) to provoke fetal movement. It is never performed during FHR decelerations or fetal bradycardia.
Educational objective:
Late decelerations of fetal
heart rate indicate
compromised fetal oxygenation. Intrauterine resuscitation interventions include administering
an IV fluid bolus, discontinuing the IV oxytocin infusion, and repositioning the client laterally.
The nurse is assigning client care activities to a licensed practical nurse (LPN) and unlicensed assistive personnel (UAP). Which of the following activities would be appropriate to assign to the LPN? Select all that apply.
| 1. Administer the daily dose of subcutaneous insulin glargine to a client. | ||
| 2. Administer a scheduled oral analgesic to a client who had surgery 2 days ago. | ||
| 3. Reinforce teaching about self-administration of insulin for a client with diabetes mellitus. | ||
| 4. Complete an admission assessment for a client admitted for an elective hysterectomy. | ||
| 5. Record client intake and output totals during the shift for all clients on the unit. |
Explanation:
| Scope of practice | ||
|---|---|---|
| RN | LPN/LVN | UAP |
|
|
|
|
*Limited assessments (eg, lung sounds, bowel sounds, neurovascular checks). LPN = licensed practical nurse; LVN = licensed vocational nurse; RN = registered nurse; UAP = unlicensed assistive personnel. |
||
Nurses preparing to delegate client care to a licensed practical nurse (LPN) and/or unlicensed assistive personnel (UAP) should consider the 5 rights of delegation. The LPN can monitor and care for stable clients who have been initially evaluated by a registered nurse (RN). Interventions that LPNs may perform include:
- Administering most medications (eg, subcutaneous insulin, oral analgesics) (Options 1 and 2)
- Reinforcing teaching and skills that have been initially taught by the RN (Option 3)
- Performing focused assessments (eg, bowel sounds) after the RN’s initial assessment
(Option 4) Performing admission or initial assessments is outside the scope of the LPN and UAP. The RN must perform initial assessments to analyze the findings and formulate the client’s plan of care before delegating tasks.
(Option 5) The LPN is capable of performing routine care (eg, calculating daily intake and output, toileting). However, the UAP may also perform these tasks, which frees the LPN to perform more complex duties. Therefore, the most appropriate staff member to assign the task of calculating intake and output is the UAP.
Educational objective:
Nurses preparing to delegate
client care should consider the 5 rights of delegation. Appropriate tasks to delegate to a
licensed practical nurse include the administration of oral and parenteral medications (excluding
those via the IV route) and reinforcement of teaching previously provided by the registered nurse.
The nurse is caring for a client with panic disorder who is reporting palpitations and intense feelings of fear. The client is shaking and hyperventilating. Which of the following actions would be a priority for the nurse to take?
| 1. Assess the client for auditory and visual hallucinations. | ||
| 2. Administer a benzodiazepine to the client. | ||
| 3. Explore possible triggers for the episode with the client. | ||
| 4. Remain in the room with the client. |
Explanation:
Panic disorder involves recurrent, brief (eg, 10- to 30-min) episodes (ie, panic attacks) during which a client experiences sudden, intense fear; anxiety; and physiological discomfort. These attacks often occur unpredictably, without an obvious trigger. Panic disorder may result from an imbalance of neurotransmitters (eg, excess norepinephrine, inadequate serotonin) or an overactivation of the amygdala.
Symptoms of a panic attack resemble many cardiac and respiratory conditions and include a fear of dying, trembling, hyperventilating, palpitations, and shortness of breath. During a panic attack, the nurse should stay with the client to promote safety and offer support (Option 4). In addition, the nurse should remain calm; use simple, clear phrases when providing instruction; and encourage the client to take slow, deep breaths if hyperventilation occurs.
(Option 1) Assessing the client for auditory and visual hallucinations may provide the nurse with information about the severity of the panic attack, but it does not ensure the client’s safety.
(Option 2) Benzodiazepines (eg, alprazolam, lorazepam) may help to calm the client, but medication should be considered only if nonpharmacological methods (eg, reducing stimuli) are unsuccessful.
(Option 3) Discussing triggers for the panic attack is not appropriate while the client is symptomatic. Once the client has calmed down, the nurse can discuss possible triggers, evaluate stressors in the client’s life, and assist in identifying prevention strategies.
Educational objective:
Panic disorder involves recurrent, brief episodes during
which a client experiences sudden, intense anxiety. During a panic attack, the nurse should
prioritize staying with the client to promote safety and offer support.
- Mental Health – Panic Disorder
The nurse is caring for a client who has a prescription for cefuroxime 30 mg/kg/day PO in 2 divided doses. The client weighs 35 lb (15.9 kg). The nurse has cefuroxime 250 mg/5 mL available. How many mL should the nurse administer to the client with each dose? Record your answer using 1 decimal place.
| Answer: (mL/dose) |
Correct Answer: 4.8 mL
Explanation:
Using dimensional analysis, perform the following steps to calculate the volume of cefuroxime in milliliters per dose:
-
Identify the prescribed, available, and required medication information
Prescribed: 30 mg cefuroxime / kg | day Available: 250 mg cefuroxime / 5 mL Required: mL / dose
-
Convert the prescription to the volume needed for administration
Prescription × available data = mL / dose
OR
( mg cefuroxime / kg | day ) ( kg / ) ( day / dose ) ( mL / mg cefuroxime ) = mL cefuroxime / dose
OR
( 30 mg cefuroxime / kg | day ) ( 15.9kg / ) ( day / 2 doses ) ( 5 mL / 250 mg cefuroxime ) = 4.77 mL cefuroxime / dose
-
Round to 1 decimal place
4.77 mL / dose ≈ 4.8 mL / dose
Educational objective:
To calculate the volume of cefuroxime in milliliters per
dose, the nurse should first identify the prescribed dose (eg, 30 mg/kg/day) and available
medication (eg, 250 mg/5 mL) and then convert to the volume in milliliters per dose (eg, 4.8 mL).
Alternative Method:
The formula method is an alternate way to calculate medication dosages. However, this method may increase the occurrence of miscalculation and medication errors. If you choose to use this method, do not round calculations until the final step.
Using the formula method, perform the following steps to calculate the volume of cefuroxime in milliliters per dose:
-
Calculate the prescribed dose in milligrams
( 30 mg cefuroxime / kg | day ) ( 15.9kg / ) ( day / 2 doses ) = 238.5 mg cefuroxime / dose
-
Convert the prescription to the volume needed for administration
Prescribed dose / available dose x available volume = mL / dose
OR
238.5 mg cefuroxime / mg cefuroxime x 5 mL = 4.77 mL cefuroxime / dose
-
Round to 1 decimal place
4.77 mL / dose ≈ 4.8 mL / dose
The nurse is caring for a client with suspected appendicitis who has vomiting and right lower quadrant pain. It would be a priority for the nurse to
| 1. administer oral pain medication | ||
| 2. obtain a urine specimen for urinalysis | ||
| 3.initiate an IV infusion of 0.9% sodium chloride | ||
| 4.obtain a blood specimen for complete blood count and serum electrolyte levels |
Explanation:
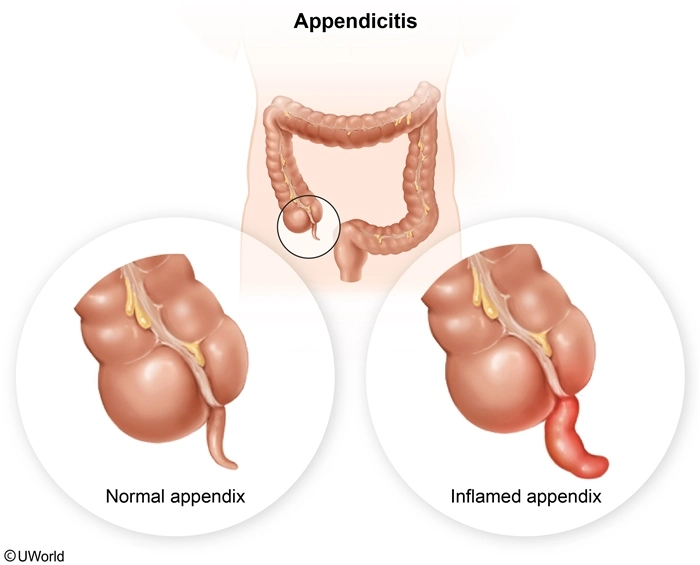
Appendicitis (ie, inflammation of the appendix) often results from obstruction by fecal matter. The obstruction traps fluid and mucus typically secreted into the colon, causing increased intraluminal pressure and inflammation. This impairs blood circulation to the appendix, resulting in swelling and ischemia. These factors increase the risk for perforation, a medical emergency that can lead to peritonitis and sepsis.
When prioritizing care of the client with appendicitis, the nurse should utilize the ABCs (ie, Airway, Breathing, Circulation). Fluid resuscitation with IV crystalloids (eg, 0.9% sodium chloride, lactated Ringer solution) is an important intervention aimed at preventing circulatory collapse resulting from fluid losses (eg, vomiting, diarrhea) and NPO status (Option 3).
(Option 1) Pain medications may be administered to promote comfort but should be administered via IV route to maintain NPO status in case of emergency surgery. In addition, circulation takes priority over pain medication.
(Options 2 and 4) Blood and urine testing often is prescribed to assist with treatment and care decisions. However, the nurse should prioritize circulatory status over obtaining laboratory specimens.
Educational objective:
Nurses caring for clients with appendicitis should
prioritize client care according to the ABCs (ie, Airway, Breathing, Circulation). Initiating
fluid resuscitation with IV crystalloids (eg, 0.9% sodium chloride) is a priority action that
prevents circulatory collapse resulting from fluid losses (eg, vomiting, diarrhea) and NPO status.
Lecture References :
- Adult Health – Appendicitis
NCLEX-style practice questions can help you identify areas needing additional study or review. Every question in our NCLEX-PN QBank includes detailed rationales for the correct and incorrect answers, so you learn as you practice.
Exhibit
The nurse auscultates the heart sounds of a 77-year-old client with chronic heart failure. Which heart sound should the nurse document? Listen to the audio clip. (Headphones are required for best audio quality.)
| 1. Pericardial friction rub | ||
| 2. S1, S2, no adventitious sounds | ||
| 3. S3 extra heart sound | ||
| 4. Systolic murmur |
Explanation:
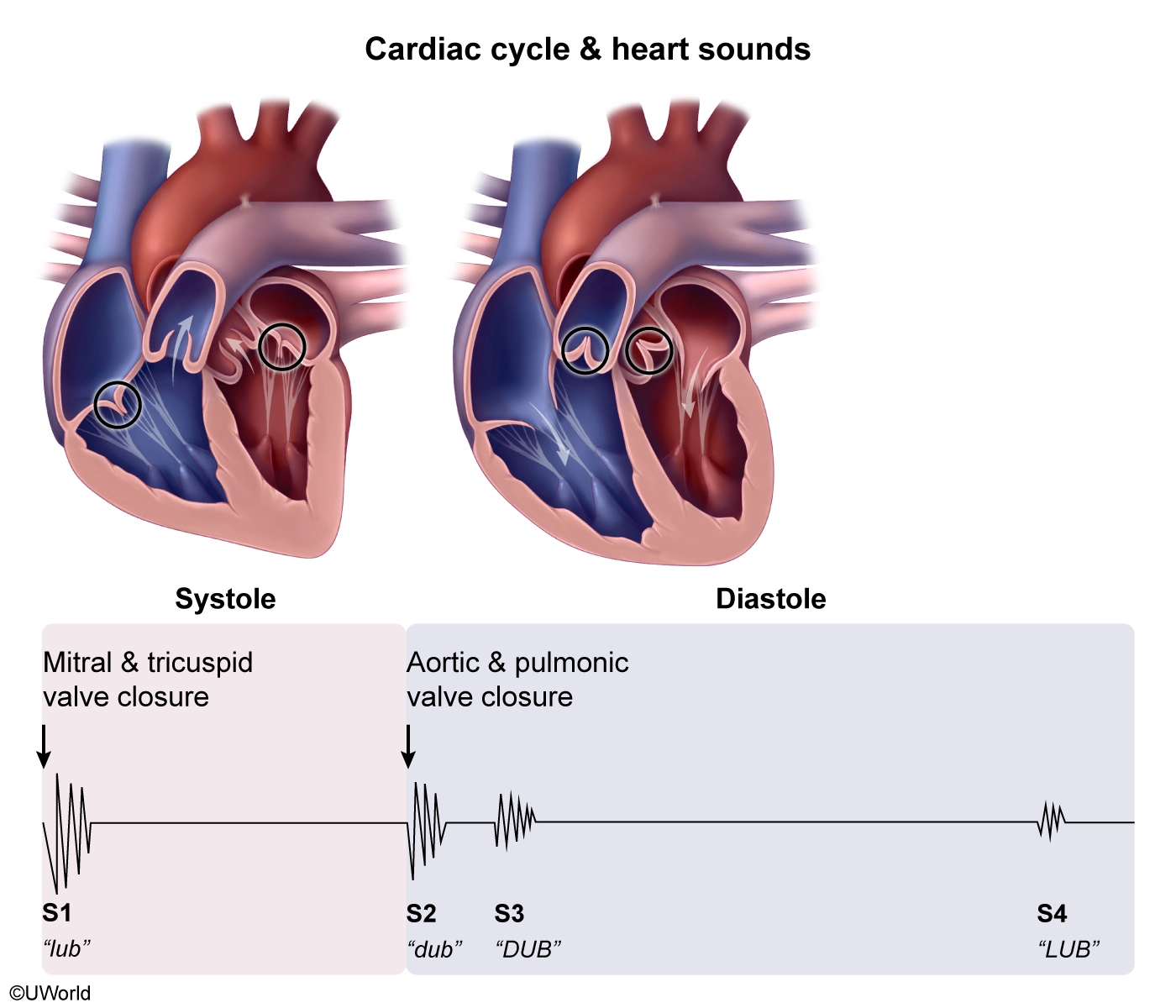
S1 and S2 are the normal “lub-dub” heart sounds that result from closure of valves. Systole occurs between S1 and S2, with S1 indicating closure of the atrioventricular (tricuspid, mitral) valves and S2 indicating closure of the pulmonic and aortic valves.
S3 is an adventitious (extra) heart sound heard as “DUB” immediately following S2 (Option 3). S3 occurs during early diastole as a result of rapid ventricular filling and is a normal finding in children and young adults. In older adults, S3 is an abnormal finding that often indicates heart failure because the sound results from decreased ventricular compliance.
S3 can be difficult to distinguish from S4. S4 is a “LUB” sound that occurs immediately before S1, during late diastole, and indicates ventricular hypertrophy.
(Option 1) A pericardial friction rub is a creaky, grating sound heard throughout systole and diastole. Friction rub occurs with pericarditis and is due to friction between inflamed layers of pericardium.
(Option 2) S1 and S2 are the normal heart sounds heard during cardiac auscultation.
(Option 4) A murmur is a swooshing, blowing, or rumbling sound caused by turbulent blood flow (eg, from valve regurgitation or stenosis).
Educational objective:
S3, the third heart sound, is a “DUB” sound that
immediately follows S2. It is a normal finding in children and young adults. S3, an
abnormal finding in older adults, often indicates heart failure.
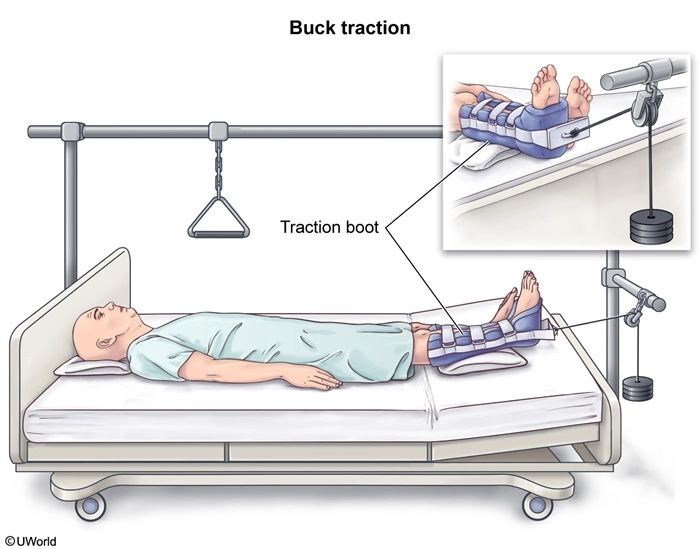
The nurse is caring for a client who has a hip fracture and is placed in Buck traction. Which of the following actions should the nurse take? Select all that apply.
| 1. Place the client on the affected side. | ||
| 2. Monitor the client for skin breakdown. | ||
| 3.Perform frequent neurovascular checks. | ||
| 4.Keep the affected extremity in a neutral position. | ||
| 5. Ensure that the client receives adequate pain relief. |
Explanation:
Buck traction is a type of skin traction used to immobilize hip fractures and reduce pain and spasm until the client can undergo surgical repair of the fracture. A traction boot is applied to the leg, below the fracture site. A weight gently and continuously pulls on the leg and hip, helping maintain alignment of the extremity. The nurse should ensure that the traction boot is fitted properly and that the extremity remains straight in a neutral position (Option 4).
Skin traction exerts pressure on the nerves, blood vessels, and soft tissue. The nurse should frequently assess the skin integrity and neurovascular status (eg, pulse, capillary refill, color, temperature, sensation, movement) of the affected extremity (Options 2 and 3). Overall pain level and efficacy of administered pain medications should be monitored closely, as increasing pain may indicate neurovascular compromise (Option 5).
(Option 1) Placing a client in Buck traction on the affected side can cause more injury. Side-to-side position changes cause the affected extremity to be adducted or abducted, which, when paired with the force of traction, can increase spasm and pain and contribute to neurovascular and orthopedic compromise.
Educational objective:
Buck traction is used to
immobilize hip fractures and reduce pain and spasm until the fracture can be repaired
surgically. Nursing interventions include frequent assessment of skin integrity and
neurovascular status; maintaining the affected extremity in a straight, neutral position; and
ensuring adequate pain relief.
Lecture References :
- Adult Health – Traction
The nurse is assigned to care for four clients. Which of the following clients should the nurse see first? Click the exhibit button for additional client information.
| 1. Female client who had an arthroscopic rotator cuff repair with sling immobilization and reports moderate swelling and tingling of the hand and fingers | ||
| 2. Female client who had an open reduction and internal fixation of the tibia and reports severe pain and pressure under the cast and inability to move the toes | ||
| 3. Male client who has two new prosthetic legs applied after traumatic, bilateral, below-the-knee amputation and reports crushing pain in the amputated areas | ||
| 4. Male client who has a hematocrit of 37% (0.37) and hemoglobin of 12.5 g/dL (125 g/L) and is prescribed enoxaparin 1 day after a total hip arthroplasty |
Explanation:
| Clinical manifestations of compartment syndrome (7 Ps) | |
|---|---|
|
Paresthesia (early sign) |
Tingling, numbness, burning |
| Pain |
Out of proportion to injury, unrelieved by medication |
| Pressure |
Taut skin, cast fits too tightly |
| Pallor |
Pale skin tone, decreased color, white, gray |
|
Pulselessness (uncommon) |
Possibly weakened or lost |
| Poikilothermy |
Cool skin temperature, matches room temperature |
|
Paralysis (late sign) |
Weakness, loss of motor activity |
Compartment syndrome occurs when swelling in a tissue compartment causes compression of arteries and nerves, typically after a direct injury (eg, fracture, dislocation) or medical device placement (eg, cast, splint). Tissue perfusion and nerve function distal to the swelling become impaired, causing signs of neurovascular compromise (eg, severe, unrelenting pain; paralysis) due to tissue ischemia. Without relieving compartment pressure (ie, cast removal, fasciotomy), ischemia leads to permanent nerve and tissue damage and/or loss of limb (Option 2).
(Option 1) Edema and numbness or tingling (paresthesia) of the hands and fingers commonly occur from inappropriate sling application. Numbness and tingling are also early signs of compartment syndrome. However, the client with late signs of compartment syndrome (eg, paralysis) should be seen first.
(Option 3) Clients with amputations may experience phantom limb pain that is severe and described as burning or crushing and requires pain management. However, limb-threatening emergencies should be managed first.
(Option 4) Slightly decreased hematocrit and hemoglobin levels are expected after hip arthroplasty due to intra- and postoperative blood loss.
Educational objective:
Compartment syndrome is a condition of impaired
circulation due to increased tissue pressure, often from edema or medical devices. Clients
with signs of compartment syndrome (eg, severe, unrelenting pain; paralysis) require immediate
assessment and intervention to prevent permanent tissue damage or loss of limb.
- Adult Health – Compartment Syndrome
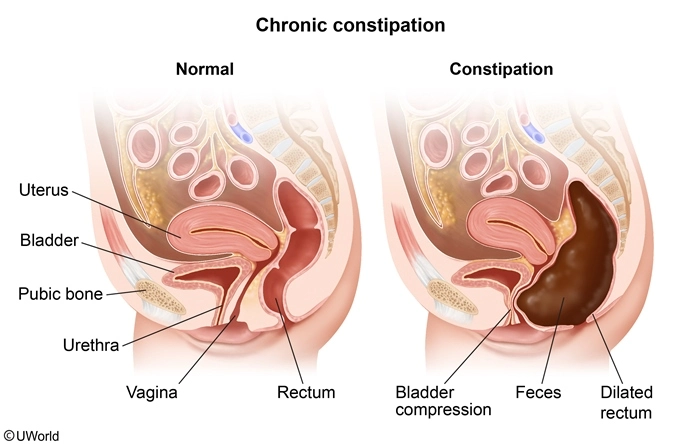
The nurse is reinforcing teaching about constipation prevention to a client. Which of the following client statements indicate appropriate understanding of the teaching? Select all that apply.
| 1. “Drinking more caffeinated drinks such as tea and soda helps to stimulate the bowel.” | ||
| 2. “Having a routine for bowel movements is important, but I should not wait if I feel the urge.” | ||
| 3. “I can use an over-the-counter laxative every other day if needed.” | ||
| 4. “I should try to eat more fruits and vegetables every day.” | ||
| 5. “Increasing my daily exercise level may help keep my bowel movements regular.” |
Explanation:
Constipation is a symptom of many disease processes (eg, Parkinson disease, diabetic neuropathy, depression), procedures (eg, abdominal surgery, bowel manipulation), and medications (eg, anticholinergics, diuretics, opioids). Immobility, low-fiber diets, decreased fluid intake, and irregular bowel habits increase the likelihood of constipation. Educate clients to prevent constipation by:
- Encouraging a healthy bowel regimen (eg, avoid delaying defecation if the urge is felt, defecate at the same time daily when possible, track bowel movements to identify changes in patterns) (Option 2)
- Increasing consumption of fruits and vegetables to reach a daily fiber intake of at least 20 g (unless contraindicated) because fiber softens and increases the bulk of stool, which promotes defecation (Option 4)
- Increasing daily exercise because activity stimulates peristalsis and promotes defecation (Option 5)
- Drinking 2-3 L of noncaffeinated fluids daily (unless contraindicated), which prevents drying and hardening of stool in the colon
(Option 1) Clients should avoid caffeinated beverages, which promote diuresis and dehydration and may lead to constipation.
(Option 3) Clients should avoid using laxatives and enemas unless prescribed by a health care provider because overuse can result in physical and psychological dependency.
Educational objective:
Constipation is a symptom of many disease processes, procedures, and medications. To prevent
constipation, educate the client to increase daily fiber intake, drink 2-3 L of fluids daily,
increase daily activity levels, and initiate a bowel regimen (eg, avoiding delay of defecation,
defecating at the same time each day).
Lecture References :
- Adult Health – Constipation
The nurse is assigning client care tasks to unlicensed assistive personnel. Which statement by the nurse is appropriate?
| 1. “I need you to take vital signs on all clients in rooms 1 through 10 this morning.” | ||
| 2.“Mrs. Jones fell out of bed during the night while walking to the commode. Please monitor her closely.” | ||
| 3. “Please ensure that Mr. Garcia in room 8 ambulates several times.” | ||
| 4. “Please take Mr. Wu’s vital signs in 10 minutes and let me know if his systolic blood pressure is &< 100.” |
Explanation:
| Five rights of delegation | |
|---|---|
| Right task |
|
| Right circumstances |
|
| Right person |
|
|
Right direction/ communication |
|
|
Right supervision/ evaluation |
|
When assigning client care, the nurse must consider the five rights of delegation. Right direction/communication involves clear and precise instructions about assigned tasks, including any specific information necessary for completion. Necessary information includes the specific tasks (eg, take vital signs), the time frame (eg, in 10 minutes), and when to report back to the nurse (eg, if systolic blood pressure is <100) (Option 4).
(Option 1) Assigning unlicensed assistive personnel (UAP) to measure vital signs “this morning” does not provide a clear time frame (eg, in 1 hour) for completion. In addition, there is no communication about what the nurse expects in terms of follow-up.
(Option 2) Instructing the UAP to monitor the client closely is an unclear direction because it does not provide specific actions to perform (eg, “Set the bed alarm.”), time intervals for performance (eg, “Check on the patient every hour.”), or criteria to report to the nurse (eg, “Notify me if the client attempts to exit the bed unassisted.”).
(Option 3) Instructing the UAP to assist with ambulation “several times” does not give a specific time frame or distance for the client to ambulate. The nurse should also communicate the conditions or aids needed to accomplish the task (eg, walks with assistance or rolling walker).
Educational objective:
Nurses assigning client care to unlicensed assistive personnel must consider the five rights of delegation. Right direction/communication involves providing clear instructions about the assigned tasks, specific information needed for task completion, the time frame, and when to report back to the nurse.
NGN Question Types & Scoring
The Next Generation NCLEX was launched on April 1, 2023 and the updated exam now contains new item types designed to better measure candidates’ clinical judgment. NCSBN also introduced a new partial credit NGN scoring model. Depending on the item type used, the 0/1 scoring rule, +/- scoring rule, or rationales scoring rule may be applied.
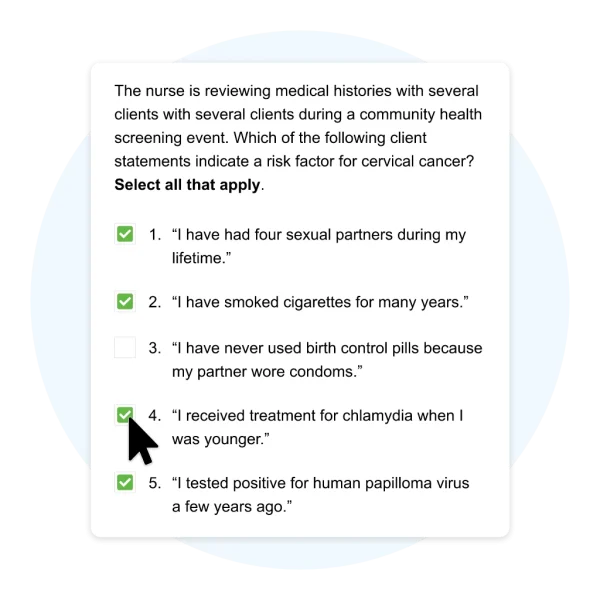
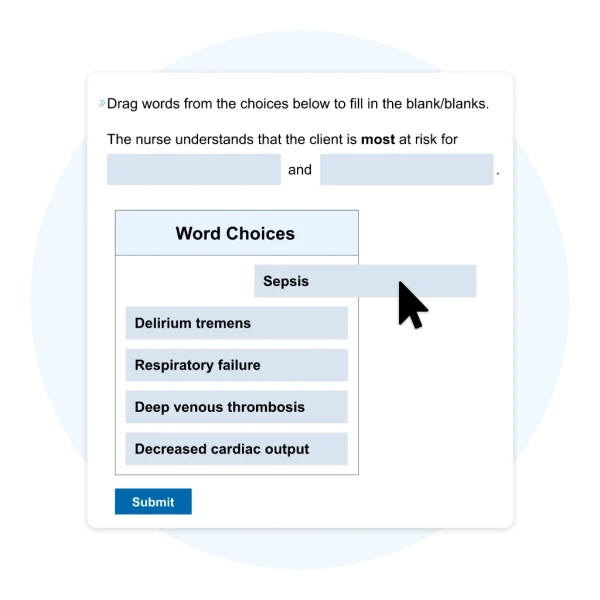
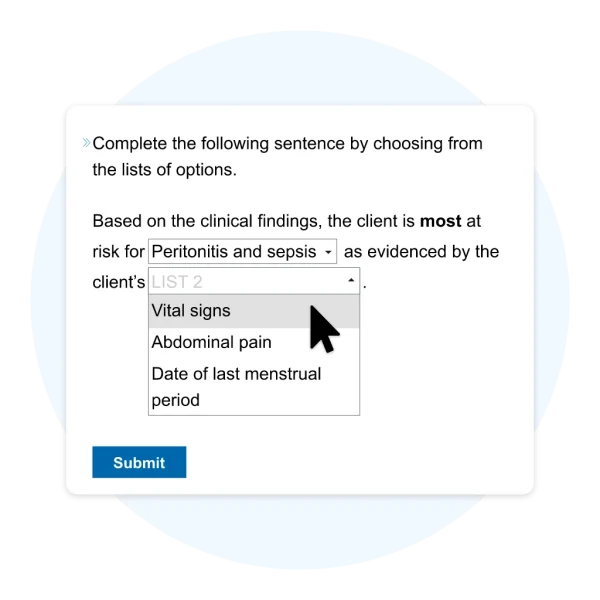
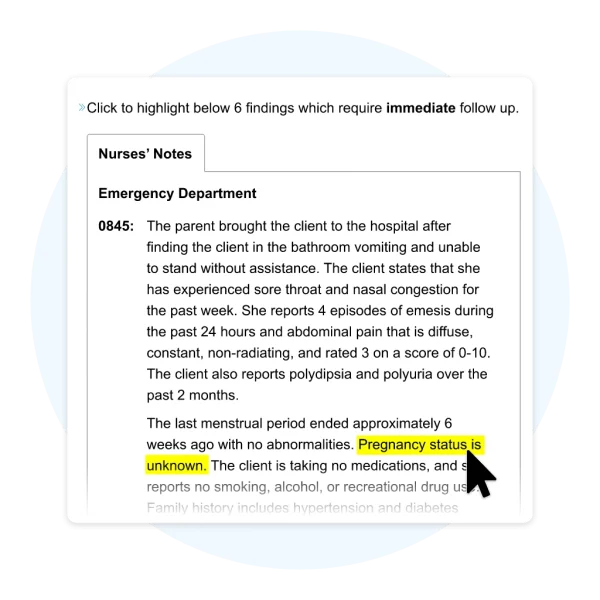
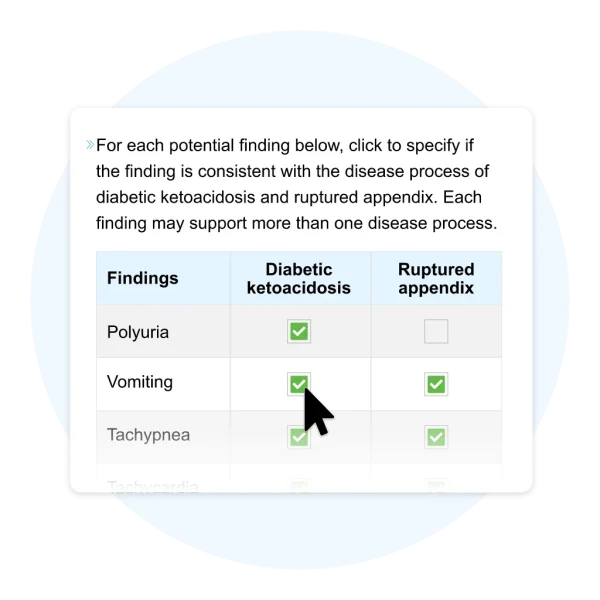
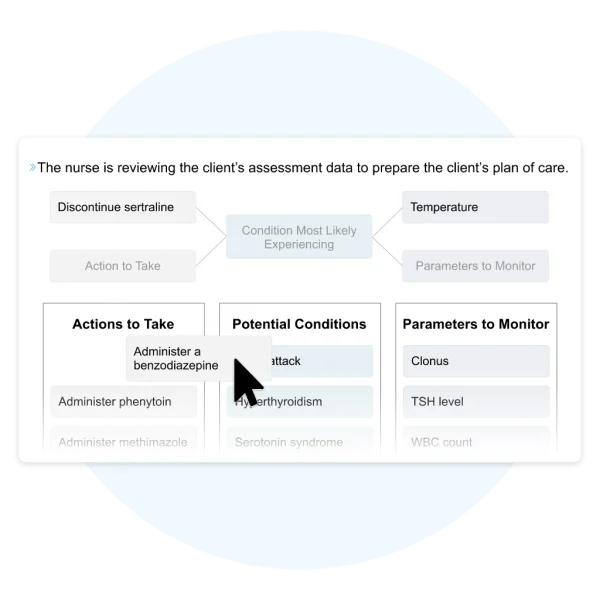
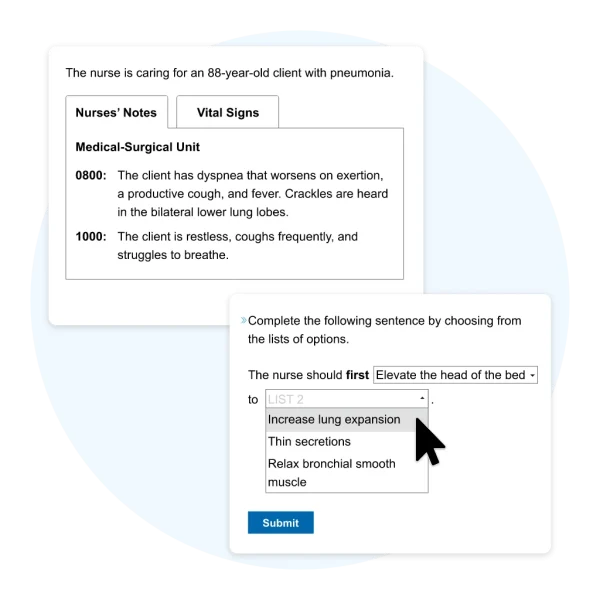
NGN Sample Questions
The future of nursing education is here. We’ve included examples below of the new NGN question types to prepare you for what’s to come.
Here’s What UWorld Nursing Students are Saying…
I love this product. I am using it in preparation for NCLEX but I wish I would have used it while I was studying in nursing school. The rationales are concise and to the point & the illustrations help with understanding the material. Great product & highly recommend it.”
UWORLD definitely prepares you for the NCLEX! The test bank is so informative and helpful! It is definitely worth getting. The rationales are amazing and go in depth with each topic. I have tried other question banks for the NCLEX and found UWORLD to be the best."
The rationales are exceptional. They really help me understand the whole picture, and then some. Reading through why the answer I chose was incorrect also helps to understand in which circumstance that answer choice would be correct.”